Cliniko now integrates with Medicare
Bulk bills and patient claims can now be processed directly from Cliniko!
Medipass co-CEO, Adrian Perillo, steps you through how, when, and who gets paid with Medicare as an Australian allied healthcare practitioner or clinic.
Adrian Perillo, Medipass·
Medicare is one of the things Australian’s are most proud of, and rightfully so. What’s not to like about publicly funded, high quality universal health care? But Medicare can be confusing and complex for the uninitiated, with lots of different claiming options and associated rules. We deal with these kinds of questions everyday at Medipass, and so in light of our new Medicare integration with Cliniko, we wanted to share an introduction to Medicare claiming, specifically for allied health providers.
The Department of Human Services (AU) has a wealth of information on Medicare claiming, spanning spending, volumes, patient demographics and more. Click here to delve into these statistics.
Interestingly, the top claimants types, by service counts, were:
While there are different rules for different conditions, most patients require a valid referral from a GP or Medical Specialist in order to claim for an allied health service. Referrals issued under the following schemes allow allied health providers and their patients to claim Medicare benefits:
Depending on the scheme, the following professions may qualify to raise claims:
Further information on these schemes can be found here.
It’s your choice as a provider whether your process bulk bill claims, patient claims, or a combination of both.
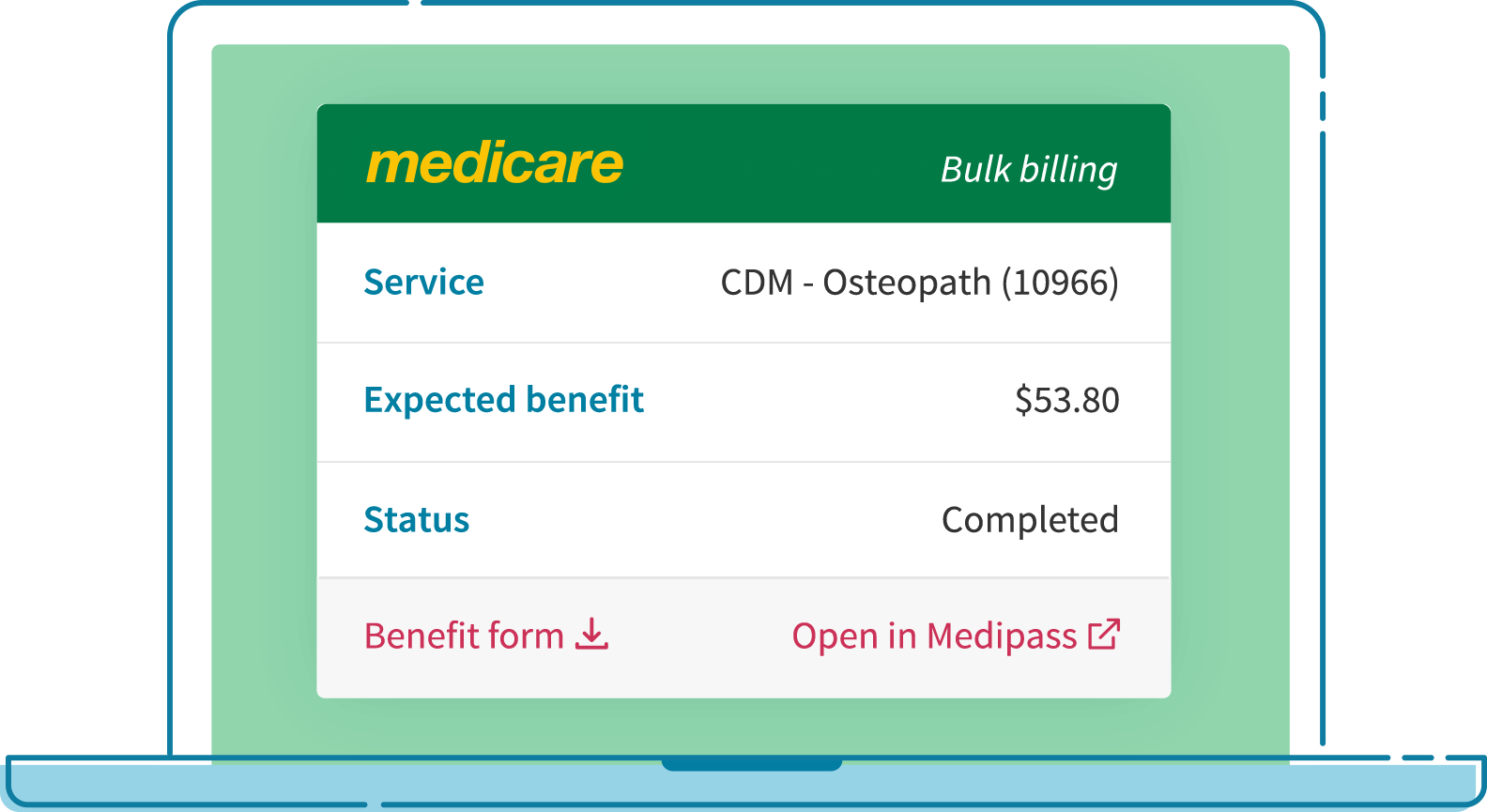
Bulk billing means the patient assigns their right to a Medicare benefit to you. In other words, Medicare pays you directly, instead of the patient. The patient doesn’t pay anything out of pocket, and Medicare pays you after you have submitted the claim on the patient’s behalf. However, bulk bill claims have a rate cap and providers cannot charge over this cap. For example, a physiotherapy session for Chronic Disease Management (CDM) typically pays the provider $53.80.
Patient claims (PCI) are when the patient or a claimant (e.g., a parent) pays you for the full amount of the service, and you lodge a Medicare claim on their behalf. If the claim is accepted, Medicare will pay the designated amount directly to the patient or claimant. It’s up to you what you charge for a patient claim service — there is no rate cap. For example, a physiotherapy session for CDM where the provider charges $100, the patient will pay the provider $100 and typically receive a benefit from Medicare of $53.80.
Overall, 86% of all Medicare claims are bulk billed. However, we have found that for allied health professionals the percentage of bulk bill claims is closer to 65%.
There are four main channels used by health professionals for Medicare (AU) claims:
It’s difficult for a patient to pay and claim for Telehealth services. Currently, common processes include:
The Medipass claiming experience is entirely online. Because Medipass doesn’t rely on hardware or terminals to process Medicare claims or out of pocket fees, it’s a perfect solution for telehealth consult claiming. Patients no longer have to manually claim with Medicare using an invoice, and it also means that there is less of an administrative burden (and you avoid potential security risks) in taking the patient’s credit card details.
When submitted during Medicare business hours, over 92% of all valid Medicare claims are approved in real-time. The remainder require Medicare review and potentially a clarification from the patient or provider. Once approved, Medicare will usually issue the benefit payment by the next business day.
For patient claims, you are paid by the patient/claimant, which could happen immediately if you accept cash. Although this means that patients/claimants are out of pocket for the entire amount, many will see a benefit payment from Medicare that same day.
If you make a successful bulk bill claim prior to 9pm Canberra time on a Medicare business day, a payment will usually be issued to you by Medicare the following business day. Claims made Saturday, Sunday and public holidays are considered as processed the following business day.
This Medicare guide was originally published on the Medipass website.
Bulk bills and patient claims can now be processed directly from Cliniko!
We get a lot of questions about the security of Cliniko , our practice management software system. I am pretty sure we get asked this question commonly because we are completely cloud-based.
This is part of an ongoing blog series that focuses on some of the fantastic features of Cliniko. Today we’re going to look at 2 Factor Authentication. What is 2 Factor Authentication (2FA)?